Diabetic neuropathy impacts roughly half of all diabetes patients, causing symptoms that range from mild discomfort to intense pain that disrupts daily activities. Patients typically experience burning, tingling, and numbness sensations that start in their feet and hands, potentially spreading to other body parts as the condition progresses.
Key Takeaways:
- One in three diabetic patients suffers from painful symptoms, with 34% experiencing moderate symptoms and 21% developing clinical neuropathy.
- Pain often gets worse at night, manifesting as sharp shooting sensations, burning feelings, and muscle weakness.
- Diabetic neuropathy appears in three primary forms: focal, polyneuropathy, and autonomic, each targeting specific body areas.
- Daily routines can be severely affected, including sleep patterns, digestive functions, and overall life quality.
- Treatment options include FDA-approved medications like pregabalin and duloxetine, plus alternative approaches such as electrical nerve stimulation to manage symptoms.
Diabetic Neuropathy Symptoms: Do I have Diabetic Neuropathy?
Common Signs and Risk Patterns
Diabetic neuropathy affects a significant portion of people with diabetes, with research showing that half of all diabetes patients develop this condition. The impact varies across different groups, hitting some harder than others. Type 2 diabetes patients, women, and South Asian populations face higher risks of developing neuropathy.
Let’s look at how symptoms typically show up:
- One in three diabetic patients experiences painful symptoms
- 34% deal with moderate symptoms in their daily lives
- 21% develop clinical neuropathy requiring medical attention
These numbers paint a clear picture of how widespread this condition is, highlighting why early detection and management are crucial. I’ve found that recognizing these patterns helps patients stay alert to early warning signs and seek timely medical attention.
Common Signs and Warning Signals
Physical Symptoms and Sensations
Diabetic neuropathy often starts with subtle changes that can worsen over time. I’ve found that pain and discomfort frequently intensify during nighttime hours, making sleep difficult for many patients. The main symptoms typically begin in the feet and hands, creating burning sensations, pins-and-needles feelings, or complete numbness that gradually moves up the limbs.
Here are the key symptoms to monitor:
- Sharp, shooting pains that may feel like electric shocks
- Burning or freezing sensations in hands and feet
- Tingling or numbness that worsens at night
- Muscle weakness, particularly in the legs
- Sudden, severe muscle cramps
- Extreme sensitivity to touch or temperature (affecting roughly 26% of patients)
These symptoms can start mild but shouldn’t be ignored. Many people mistake early signs for normal aging or fatigue, but early recognition leads to better management. Muscle weakness often affects daily activities like walking or holding objects, while sensory changes can make it harder to feel temperature differences or minor injuries. If you notice any of these signs, especially if they’re persistent or worsening, it’s important to consult a healthcare provider for proper evaluation and treatment options.
Types of Nerve Damage in Diabetic Patients
Understanding Different Neuropathy Patterns
Nerve damage from diabetes can affect different parts of your body in distinct ways. Here’s a breakdown of the three main types of diabetic neuropathy you might experience.
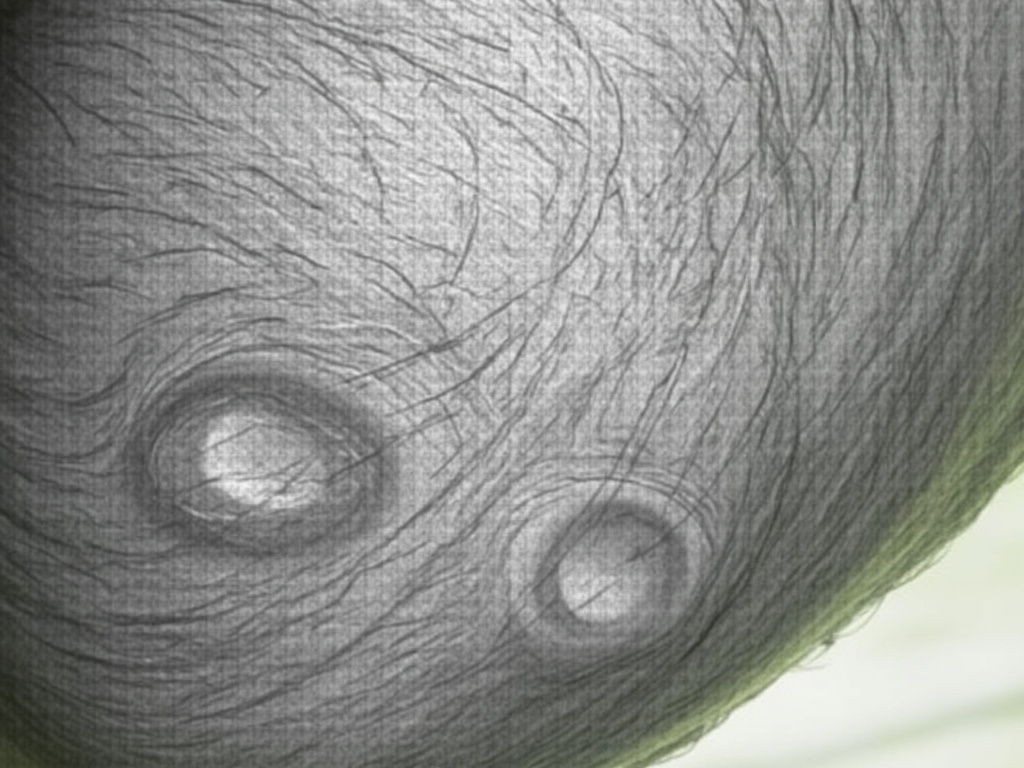
Focal neuropathy targets individual nerves, causing sudden pain or weakness in specific areas. This can impact your:
- Eye muscles, leading to double vision
- Facial muscles, resulting in Bell’s palsy
- Chest area, creating pain that might feel like a heart attack
Diabetic polyneuropathy affects multiple nerves throughout your body, particularly in your feet and legs. Common signs include:
- Tingling or burning sensations in your feet
- Numbness that gradually moves up your legs
- Sharp pains, especially at night
- Loss of balance and coordination
Autonomic neuropathy affects the nerves controlling your internal organs. You might notice:
- Digestive problems like bloating or nausea
- Irregular heart rate
- Changes in blood pressure
- Bladder control issues
- Excessive or reduced sweating
Each type of neuropathy can show up on its own or combine with others, making early recognition crucial. I recommend paying attention to any new sensations or changes in your body and discussing them with your healthcare provider promptly.

Impact on Daily Life and Body Functions
Sleep and Quality of Life Changes
Living with diabetic neuropathy can significantly affect sleep patterns and daily activities. Burning or tingling sensations often intensify at night, making restful sleep difficult. This creates a cycle of fatigue that impacts work performance and social interactions.
Autonomic System Disruptions
Neuropathy doesn’t just affect nerves in your feet and hands – it can disturb your entire autonomic nervous system. Here are common ways it affects bodily functions:
- Digestive problems like frequent nausea, unexpected vomiting, and persistent constipation
- Sexual health issues including reduced sensation and erectile dysfunction
- Irregular sweating that leads to skin problems and temperature control issues
- Unstable blood pressure, especially when standing up quickly
- Bladder control difficulties and increased urination frequency
These symptoms vary in severity, but early recognition helps manage them effectively. I recommend tracking new symptoms as they appear to discuss with your healthcare provider.
Treatment Options and Medications
Prescription Medications
The FDA has given its stamp of approval to two primary medications for diabetic neuropathy: pregabalin (Lyrica) and duloxetine (Cymbalta). These medications work by calming overactive nerves and reducing pain signals to the brain. I’ve found that doctors often start with these options due to their proven track record.
Alternative Treatment Approaches
Beyond FDA-approved options, several other medications have shown promise in managing neuropathy symptoms:
- Gabapentin helps reduce nerve pain and can improve sleep quality
- Amitriptyline, an older antidepressant, can lessen nighttime discomfort
- Venlafaxine and desvenlafaxine target both pain and mood-related symptoms
- Lidocaine 5% patches provide targeted relief for specific painful areas
- Capsaicin cream creates a warming sensation that can interrupt pain signals
- Isosorbide dinitrate spray can improve blood flow to affected areas
I’ve seen electrical nerve stimulation emerge as a helpful complementary therapy. It’s particularly useful for people who prefer non-medication approaches or need additional pain relief. This treatment sends mild electrical pulses through the skin to disrupt pain signals and can be done at home with a portable unit.
Remember, these treatments often work best when combined with good blood sugar control. Your doctor can create a personalized plan based on your symptoms and overall health status.
Sources:
Johns Hopkins Medicine
Diabetes Journals
American Academy of Family Physicians
Better Health Victoria
Health Direct Australia