Peripheral neuropathy, a condition impacting millions worldwide, arises from damage to the peripheral nervous system—the intricate network of nerves extending beyond the brain and spinal cord. This comprehensive report delves into the diverse causes of peripheral neuropathy, ranging from common culprits like diabetes to less prevalent factors such as genetic mutations, exposure to toxins, and in some cases, unknown causes. Understanding these causes is crucial for effective prevention, diagnosis, and management of this often debilitating condition.
Prevalence and Significance
Peripheral neuropathy affects approximately 2.4% of the global population, with the prevalence rising to 8% in older adults. In the United States alone, an estimated 20 million people suffer from this condition. Diabetic neuropathy is a highly prevalent form, occurring in approximately half of individuals with diabetes. It’s important to note that a significant portion of neuropathy cases are idiopathic, meaning the cause remains unknown even after extensive evaluation. Leprosy is another notable cause, remaining a significant contributor to peripheral neuropathy globally, particularly in Southeast Asia. The substantial impact of peripheral neuropathy on individuals and healthcare systems underscores the importance of understanding its diverse etiologies.
Research Methodology
This report draws on a wide range of medical literature to provide a comprehensive overview of the causes of peripheral neuropathy. The information presented is based on peer-reviewed medical articles, reputable medical websites, and research papers on the scientific mechanisms and higher-level causes of neuropathy.
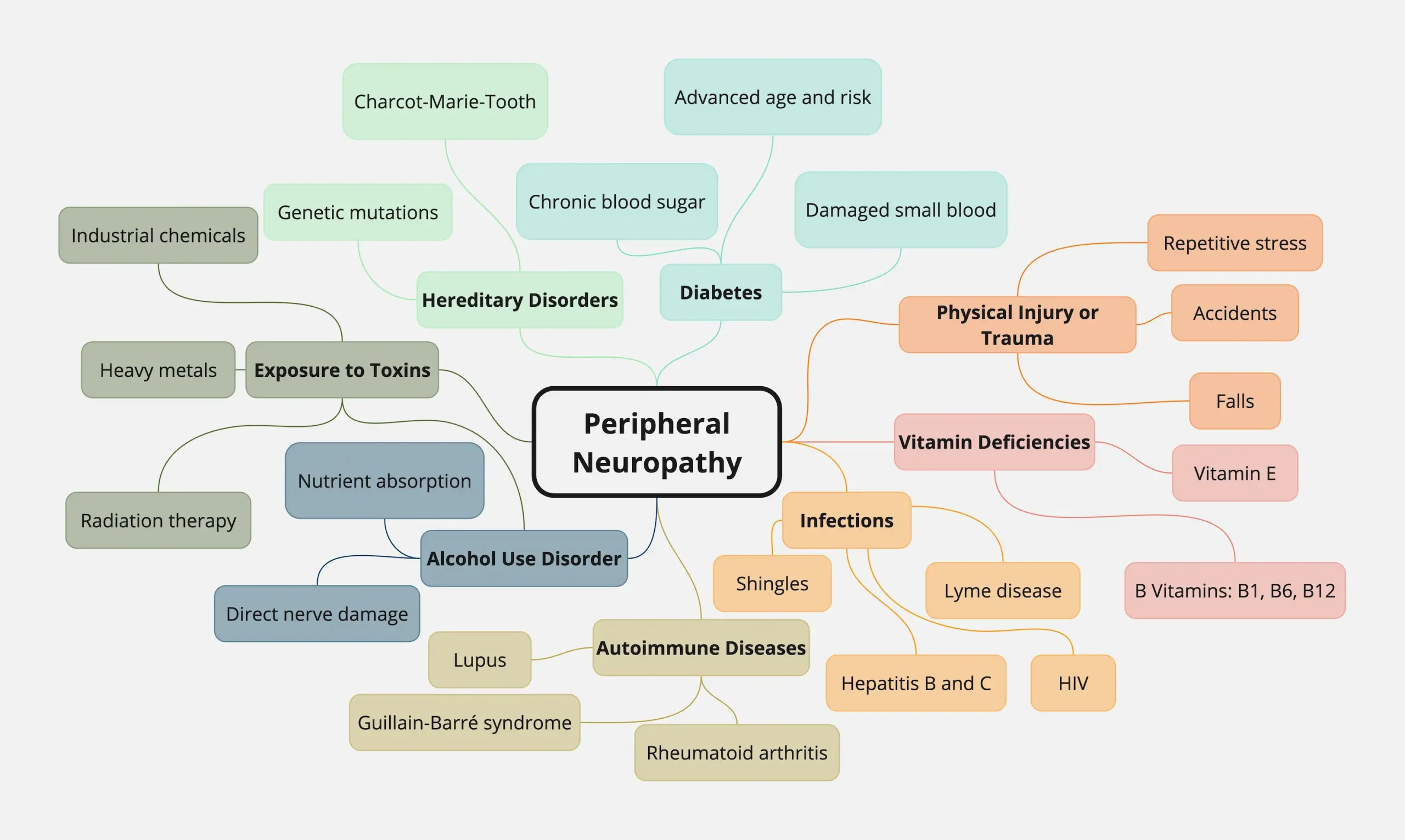
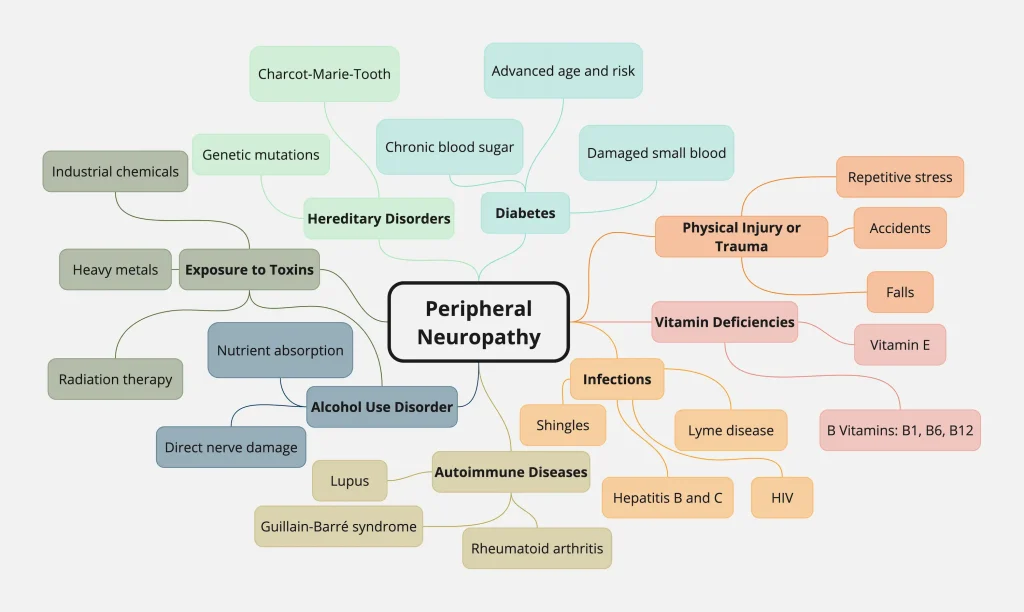
Causes of Peripheral Neuropathy
| Cause | Description | Example Conditions/Factors |
|---|---|---|
| Diabetes | Chronically elevated blood sugar levels damage small blood vessels that supply nerves, leading to nerve fiber damage and dysfunction. | Type 1 and Type 2 diabetes |
| Alcohol Use Disorder | Excessive alcohol consumption can directly damage nerves and interfere with nutrient absorption, contributing to neuropathy. | Alcoholism |
| Vitamin Deficiencies | Inadequate intake or absorption of essential vitamins, especially B vitamins and vitamin E, can disrupt nerve function. | Deficiencies in B1, B6, B12, and vitamin E |
| Autoimmune Diseases | The immune system mistakenly attacks the body’s own tissues, including peripheral nerves, causing inflammation and damage. | Rheumatoid arthritis, lupus, Guillain-Barré syndrome |
| Infections | Certain infections can directly damage nerves or trigger an immune response that leads to nerve damage. | Lyme disease, shingles, HIV, hepatitis B and C |
| Kidney and Liver Disorders | Kidney and liver diseases can impair the body’s ability to filter toxins, leading to nerve damage from accumulated toxins. | Chronic kidney disease, cirrhosis |
| Exposure to Toxins | Exposure to heavy metals, industrial chemicals, certain medications (including chemotherapy), and radiation therapy can damage nerves. | Lead, mercury, arsenic, industrial solvents, chemotherapy drugs, radiation exposure |
| Physical Injury or Trauma | Physical injuries, nerve compression, and repetitive stress from certain activities can damage peripheral nerves. | Accidents, falls, surgeries, carpal tunnel syndrome, playing musical instruments, using vibrating tools |
| Hereditary Disorders | Genetic mutations inherited from parents can cause various forms of peripheral neuropathy. | Charcot-Marie-Tooth disease |
| Medications | Certain medications can cause peripheral neuropathy as a side effect. | Chemotherapy drugs, medications for HIV/AIDS |
| Amyloidosis | Abnormal protein buildup in organs can affect the nervous system, leading to peripheral neuropathy. | Various types of amyloidosis |
Diabetes
Diabetes is the leading cause of peripheral neuropathy, particularly when blood sugar levels are poorly managed. Chronically elevated blood sugar levels damage the small blood vessels that supply nutrients and oxygen to the peripheral nerves, leading to nerve fiber damage and dysfunction. This damage typically affects the nerves in the feet and legs first, causing symptoms such as numbness, tingling, and pain. Several risk factors increase the likelihood of developing diabetic neuropathy, including advanced age, hypertension, peripheral vascular disease, smoking, dyslipidemia, poor glucose control, long-standing diabetes, obesity, and excessive alcohol consumption.
Alcohol Use Disorder
Excessive alcohol consumption over prolonged periods can directly damage peripheral nerves . Alcohol can also interfere with the absorption of essential nutrients like vitamin B12, which is crucial for nerve health. This deficiency further contributes to nerve damage and the development of peripheral neuropathy.
Vitamin Deficiencies
Inadequate intake or absorption of certain vitamins, particularly B vitamins (B1, B6, B12) and vitamin E, can contribute to peripheral neuropathy . These vitamins play vital roles in nerve function and maintenance. Deficiencies can disrupt nerve signaling and lead to a range of symptoms, including numbness, tingling, and muscle weakness.
Autoimmune Diseases
Autoimmune diseases, such as rheumatoid arthritis, lupus, and Guillain-Barré syndrome, can trigger peripheral neuropathy . In these conditions, the immune system mistakenly attacks the body’s own tissues, including the peripheral nerves. This immune attack can cause inflammation and damage to the nerves, leading to neuropathy.
Infections
Certain infections, including Lyme disease, shingles, HIV, and hepatitis B and C, can cause peripheral neuropathy. These infections can directly damage the nerves or trigger an immune response that leads to nerve inflammation and damage.
Kidney and Liver Disorders
Kidney and liver diseases can disrupt the body’s ability to filter toxins, leading to the accumulation of harmful substances in the blood that can damage peripheral nerves. This damage can cause a range of neuropathic symptoms.
Exposure to Toxins
Exposure to various toxins, including heavy metals (lead, mercury, arsenic), industrial chemicals, and certain medications (chemotherapy drugs), can cause peripheral neuropathy. These toxins can directly damage nerve tissue or interfere with nerve function. Radiation therapy, used in cancer treatment, can also cause nerve damage, with symptoms sometimes appearing months or years after exposure.
Physical Injury or Trauma
Physical injuries, such as those sustained in accidents, falls, or surgeries, can damage peripheral nerves . Nerve compression or entrapment, as seen in carpal tunnel syndrome, can also lead to neuropathy. Repetitive stress from certain jobs or hobbies, such as playing musical instruments or using vibrating tools, can also put pressure on peripheral nerves and cause damage.
Hereditary Disorders
Some forms of peripheral neuropathy are inherited, meaning they are caused by genetic mutations passed down from parents to their children. Charcot-Marie-Tooth disease is a common example of hereditary neuropathy. It’s important to note that even within the same inherited neuropathy, different genetic mutations can lead to varying clinical presentations, highlighting the complexity of genetic factors in this condition.
Medications
Certain medications, particularly those used to treat cancer (chemotherapy), HIV/AIDS, and other conditions, can cause peripheral neuropathy as a side effect.
Amyloidosis
Amyloidosis, a condition characterized by the abnormal buildup of proteins in organs, can also lead to peripheral neuropathy. These protein deposits can affect the nervous system, causing nerve damage and a range of neuropathic symptoms.
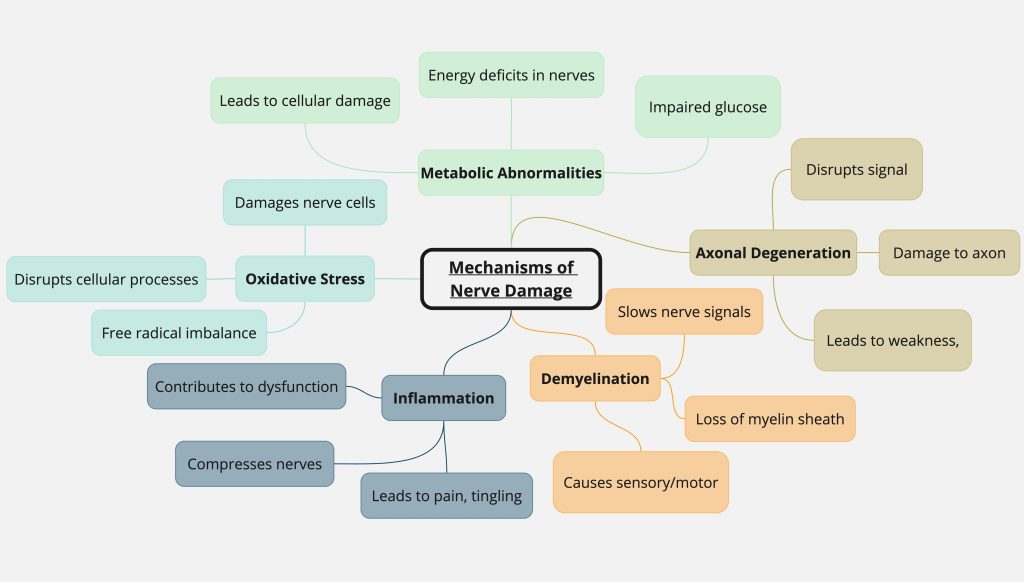
Scientific Mechanisms of Peripheral Neuropathy
The underlying mechanisms of peripheral neuropathy vary depending on the cause. However, some common pathways involved in nerve damage include:
- Axonal Degeneration: Damage to the axon, the long, slender projection of a nerve cell that transmits signals, is a common feature in many neuropathies . This damage can disrupt or completely block nerve signal transmission, leading to muscle weakness, numbness, and other symptoms.
- Demyelination: The myelin sheath is a protective covering around nerve fibers that helps with efficient signal transmission. Demyelination, or the loss of this sheath, can slow down or block nerve signals, similar to the effect of damaged insulation on an electrical wire. This can result in a variety of sensory and motor problems.
- Inflammation: Inflammation of the nerves or surrounding tissues can contribute to nerve damage and dysfunction. Inflammatory processes can compress or irritate nerves, leading to pain, tingling, and other symptoms.
- Oxidative Stress: An imbalance between free radicals and antioxidants in the body can lead to oxidative stress, which can damage nerve cells. This damage can disrupt cellular processes and contribute to nerve dysfunction.
- Metabolic Abnormalities: Metabolic disorders, such as diabetes, can disrupt the normal metabolic processes in nerve cells, leading to nerve damage. This can involve impaired glucose metabolism, leading to energy deficits and cellular damage in nerves.
Higher-Level Causes of Peripheral Neuropathy
In addition to the specific causes mentioned above, several higher-level factors can increase the risk of developing peripheral neuropathy:
Lifestyle Factors
- Excessive alcohol consumption: As discussed earlier, alcohol can directly damage nerves and contribute to nutritional deficiencies that worsen neuropathy.
- Poor nutrition: A diet lacking essential vitamins and nutrients can impair nerve health and increase susceptibility to neuropathy.
- Lack of physical activity: Physical inactivity can contribute to various health problems, including diabetes and obesity, which are risk factors for peripheral neuropathy.
- Hormonal imbalances: Hormonal imbalances can disturb the body’s metabolic processes and cause tissue swelling that presses on peripheral nerves, potentially leading to neuropathy.
Environmental Factors
- Exposure to toxins: Exposure to environmental toxins, such as heavy metals and industrial chemicals, can directly damage nerves.
Genetic Factors
- Inherited genetic mutations: As mentioned earlier, certain genetic mutations can increase the risk of developing specific types of peripheral neuropathy.
Diagnostic Criteria and Differential Diagnosis
Diagnosing peripheral neuropathy involves a comprehensive evaluation, including:
- Medical History: A detailed medical history, including any underlying medical conditions, medications, and lifestyle factors, is crucial.
- Physical Examination: A neurological examination to assess reflexes, sensation, and muscle strength.
- Nerve Conduction Studies and Electromyography: These tests measure the electrical activity of nerves and muscles to assess nerve damage.
- Blood Tests: To identify underlying medical conditions, such as diabetes or vitamin deficiencies.
- Nerve Biopsy: In some cases, a nerve biopsy may be performed to examine nerve tissue under a microscope.
It’s important to differentiate peripheral neuropathy from other conditions with similar symptoms, such as radiculopathy (pinched nerve in the spine) and myelopathy (spinal cord disease).
Conclusion
Peripheral neuropathy is a complex condition with a wide range of causes, from common culprits like diabetes to less prevalent factors like genetic mutations and exposure to toxins. Importantly, a significant number of cases are idiopathic, with no identifiable cause. The underlying mechanisms of nerve damage are diverse, involving axonal degeneration, demyelination, inflammation, oxidative stress, and metabolic abnormalities. Higher-level factors, such as lifestyle choices, environmental exposures, and genetic predispositions, also play a role in the development of peripheral neuropathy.
The interconnectedness of these various causes highlights the challenges in diagnosing and managing this condition. A holistic approach, considering all potential contributing factors, is crucial for effective prevention and treatment. Early diagnosis and appropriate interventions are essential to minimize the impact of peripheral neuropathy on patients’ quality of life.
Sources
1. Neuropathy – StatPearls – NCBI Bookshelf, accessed January 13, 2025, https://www.ncbi.nlm.nih.gov/books/NBK542220/
2. What Is Peripheral Neuropathy? – American Brain Foundation, accessed January 13, 2025, https://www.americanbrainfoundation.org/diseases/peripheral-neuropathy/
3. Peripheral neuropathy – Causes – NHS, accessed January 13, 2025, https://www.nhs.uk/conditions/peripheral-neuropathy/causes/
4. People’s experiences living with peripheral neuropathy: a … – Frontiers, accessed January 13, 2025, https://www.frontiersin.org/journals/pain-research/articles/10.3389/fpain.2023.1162405/full
5. Peripheral Neuropathy | National Institute of Neurological Disorders and Stroke, accessed January 13, 2025, https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy
6. Diabetic peripheral neuropathy: pathogenetic mechanisms and treatment – Frontiers, accessed January 13, 2025, https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1265372/full
7. Types of Risk Factors – The Foundation For Peripheral Neuropathy, accessed January 13, 2025, https://www.foundationforpn.org/types-risk-factors/
8. Peripheral neuropathy – Symptoms and causes – Mayo Clinic, accessed January 13, 2025, https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
9. Diabetic Peripheral Neuropathy – StatPearls – NCBI Bookshelf, accessed January 13, 2025, https://www.ncbi.nlm.nih.gov/books/NBK442009/
10. Causes of Peripheral Neuropathy | the Foundation for PN, accessed January 13, 2025, https://www.foundationforpn.org/causes/
11. Peripheral Neuropathy: What It Is, Symptoms & Treatment – Cleveland Clinic, accessed January 13, 2025, https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
12. www.mayoclinic.org, accessed January 13, 2025, https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061#:~:text=Peripheral%20neuropathy%20is%20nerve%20damage,inflammatory%20demyelinating%20polyneuropathy%20and%20vasculitis.
13. Peripheral Neuropathy | NINDS Catalog, accessed January 13, 2025, https://catalog.ninds.nih.gov/sites/default/files/publications/peripheral-neuropathy.pdf
14. Peripheral Neuropathy – Symptoms, Types and Causes – WebMD, accessed January 13, 2025, https://www.webmd.com/brain/understanding-peripheral-neuropathy-basics
15. Can neuropathy be a hereditary condition? – MedicalNewsToday, accessed January 13, 2025, https://www.medicalnewstoday.com/articles/is-neuropathy-hereditary
16. Diseases which cause generalized peripheral neuropathy: a systematic review – PubMed, accessed January 13, 2025, https://pubmed.ncbi.nlm.nih.gov/34214006/
17. PERIPHERAL NEUROPATHY, accessed January 13, 2025, https://www.urmc.rochester.edu/MediaLibraries/URMCMedia/center-experiential-learning/cme/types-of-activities/documents/PERIPHERAL-NEUROPATHY-HANDOUT.pdf